 Getty Images
Getty ImagesMore than one million extra women could have life-saving cervical-cancer checks if the NHS adopted do-it-yourself testing, researchers estimate.
The team at King’s College London said the results of its self-testing trial were “fantastic” and “gave power to women”.
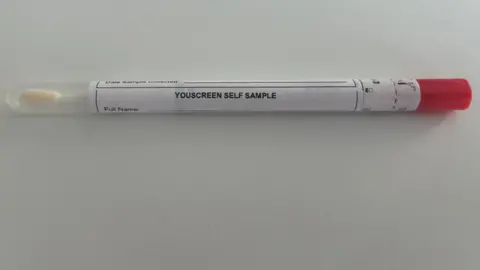
The kits are like a Covid swab but longer and are posted to a lab for analysis.
The NHS called the findings extremely positive and is assessing whether to roll out the scheme.
There are more than 3,000 new cases of cervical cancer in the UK each year.
The cervix is the small opening joining the top of the vagina to the base of the womb.
‘Uncomfortable experience’
Women are invited for cervical-cancer screening – what used to be known as the smear test – every three to five years between the ages of 25 and 65.
But about 4.6 million women in England – nearly a third of those offered screening – do not come forward.
“Cervical cancer screening has been in decline for the last 20 years,” a senior consultant on the trial, Mairead Lyons, said.
“Many women will describe it as an uncomfortable experience [or they are] too busy, embarrassed or afraid of the physical experience of it.”
The YouScreen trial is the first time self-testing has been offered as part of cervical-cancer screening in the UK.
Women, and people with a cervix, were offered a self-testing kit in one of two ways:
- If they were six months overdue for screening and went to their GP for any reason, their doctor would be automatically alerted and offer a kit
- If they were 15 months overdue for screening, a kit was sent to their home address
 YouScreen
YouScreenThe kit contains a long cotton-wool bud, used to swab the lining of the vagina for about 20 seconds.
This is sent to a laboratory to test for human papillomavirus (HPV) which causes most cervical cancers.
If this is positive, they are invited for a further test to see if any cells in the cervix have started the journey to becoming a cancer.
The trial ran in five London boroughs, in 2021, and 27,000 test kits were offered.
The results, published in eClinicalMedicine, showed:
- 56% completed tests offered by their GP
- 13% completed tests posted to their home
If these results were replicated across the whole of England, the researchers estimate it would increase the proportion screened from 69.9% to 77.3% – about one million extra women over a three-year screening cycle.
The trial also showed self-testing reached women irrespective of their ethnicity or wealth.
‘A game-changer’
“I am so excited by it,” Ms Lyons told me.
“I’ve spent over 30 years in the health service and this is fantastic.”
Dr Anita Lim, from King’s College London, said: “Self-sampling has been hailed as a game-changer for cervical screening – and we now have evidence in a UK population to show that it really is.”
Self-testing is already offered in Australia, the Netherlands, Denmark and Sweden.
NHS England screening and vaccination director Deborah Tomalin called the trial results “extremely promising”.
“The NHS will now be working with the UK National Screening Committee to consider the feasibility of rolling this out more widely across England,” she said.
Meanwhile, the HPV vaccine is cutting cervical cancer by nearly 90%.
And Prof Peter Sasieni, who was also involved in the self-testing trial, said young women who had had the HPV vaccine in childhood may need only one to three cervical cancer screenings in their lifetime.
No changes to the screening programme for vaccinated women have yet been made so the advice is to attend when invited for screening.
But he added: “Unfortunately, women born before 1990 are unlikely to benefit from the HPV vaccine, so regular screening is vitally important to protect those who have not been vaccinated.”
Main symptoms of cervical cancer
- vaginal bleeding that’s unusual for you – including during or after sex, between periods or after the menopause – or heavier periods than usual
- changes to vaginal discharge
- pain during sex or in the lower back, lower tummy or between the hip bones (pelvis)
Source: NHS





