 Cheshire Constabulary
Cheshire ConstabularyJunior doctors referred to Lucy Letby as “Nurse Death”, a public inquiry has heard.
The Thirlwall inquiry, set up to examine the NHS response to the serial killer, heard the head of nursing told a review into increased baby deaths that paediatricians thought Letby was “the common denominator”.
Nicholas de la Poer KC, on behalf of the counsel for the inquiry, also told the hearing Letby had attempted to murder one of the babies during a hospital inspection.
The 34-year-old was convicted of murdering seven babies and attempting to murder another seven at the Countess of Chester Hospital between June 2015 and June 2016.
Ian Harvey, the medical director at the trust, discussed concerns about Letby in an interview with an external review team in September 2016, the inquiry heard.
Notes from his interview shared at the hearing said paediatricians saw Letby as the “elephant in the room”.
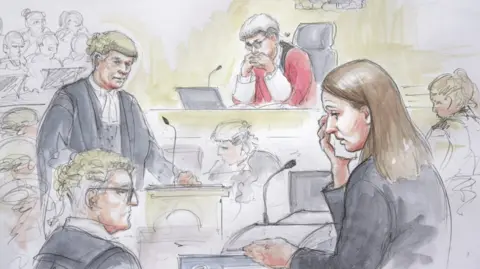 Helen Tipper
Helen TipperMr Harvey was also noted to say he had to “intervene with the neonatal lead as junior doctors had been referring to her as ‘Nurse Death’.”
His notes continued: “Ripples through the team and trying to function. Can’t see how to conclude without calling the police.
“Unless there is something to satisfy the medical staff they can call the police.”
Mr de la Poer told the inquiry that Mr Harvey also said “need to pull together before we press the nuclear button” when asked what the “tipping point” was before taking matters to the police.
Head of nursing Alison Kelly told the review team that paediatricians thought Letby was the “common denominator”, adding there were no issues with her competency.
She also said: “Clinicians threatened to go to the police.”
The inquiry has heard Cheshire Police was not contacted until May 2017, while the trust also failed to make a referral to other regulatory agencies including the Nursing and Midwifery Council.
 Cheshire Constabulary
Cheshire ConstabularyThe trust discussed the matter informally with a senior Cheshire Police officer at a meeting on 27 April, 2017.
Det Ch Supt Nigel Wenham, of Cheshire Police, told the inquiry that the term “angel of death” was used at the meeting to describe Letby.
He briefed senior officers at Cheshire Police on 2 May that year, and the force planned to obtain a letter from the hospital formally inviting them investigate unexplained deaths on the neonatal unit.
Even after this point, Mr Harvey told NHS England that consultants from the neonatal unit had influenced the police by sending a letter “which was a very prejudiced view, effectively pointing the finger at one nurse.”
He stated that his “own feeling” was that there would not be an investigation unless there was something “new” disclosed by the doctors.
He added that he believed the force would assist the trust “in a message that will allow us to close down the speculation here and deal with the issues of culture.”
In fact, the consultants sat down with the police on 17 May, 2017, and outlined in detail why they believed the deaths were suspicious.

Mr de la Poer said Det Ch Supt Wenham described this meeting as a “critical and important event”.
That afternoon Cheshire Police decided there were sufficient grounds to suspect a criminal offence and to launch a criminal investigation.
Mr de la Poer also addressed the role of the Car Quality Commission healthcare watchdog (CQC), which was in the process of inspecting the hospital the same day Letby tried to kill a baby.
Letby was convicted of trying to murder the child, referred to in court as Baby K, by dislodging her breathing tube and leaving her to deteriorate in March 2016.
Mr de la Poer said the lead consultant on the neonatal unit, Dr Stephen Brearey, stated that “neonatal mortality was not brought up” by inspectors.
He said one of his colleagues told them that staff had “serious patient safety concerns and don’t feel like we are being listened to” but was ignored.
The inspectors left before there was time to expand upon the concerns, Mr de la Poer added.
‘Reputational risk’
The inquiry heard one of the CQC inspectors, Elizabeth Childs, did not recall having a discussion about increased, unexpected or unexplained neonatal deaths during the inspection.
The hearing was also told that a spike in the number of babies who died at the Countess of Chester was missed by regional hospital bosses.
Clinicians had failed to appreciate a “stark” difference in infant mortality data, Mr de la Poer told the inquiry.
Statistics showing that baby deaths rose from three in a year to eight in nine months between 2014 and 2015 were presented to a steering group of the Cheshire and Merseyside Neonatal Network in January 2016, he said.
But concerns about the increased number of baby deaths were only logged on the trust’s urgent care risk register in July of that year.
However, the risk was categorised as “potential damage to the reputation” of the unit and the hospital – rather than a risk to the safety of babies on that ward.





